Sore throats are extremely common, and are often associated with a high temperature.
- In young children, sore throats are most commonly caused by viral infections – if this is the case, your child is likely to also have a runny nose, cough or earache. However, there are currently high circulating rates of a bacteria called Strep A - if your child is unwell with a fever, severe sore throat, pus on their tonsils (at the back of their throat) and hasn't got viral symptoms such as a runny nose, they may need treatment with antibiotics. If they also have a red tongue, swollen/painful glands in their neck and a sandpaper rash, they may have scarlet fever - in this case, please arrange for them to be seen by a healthcare professional as they are likely to need treatment with antibiotics.
- If a number of people are unwell in the same household, this also suggests a viral infection (because viral infections spread more easily than bacterial infections).
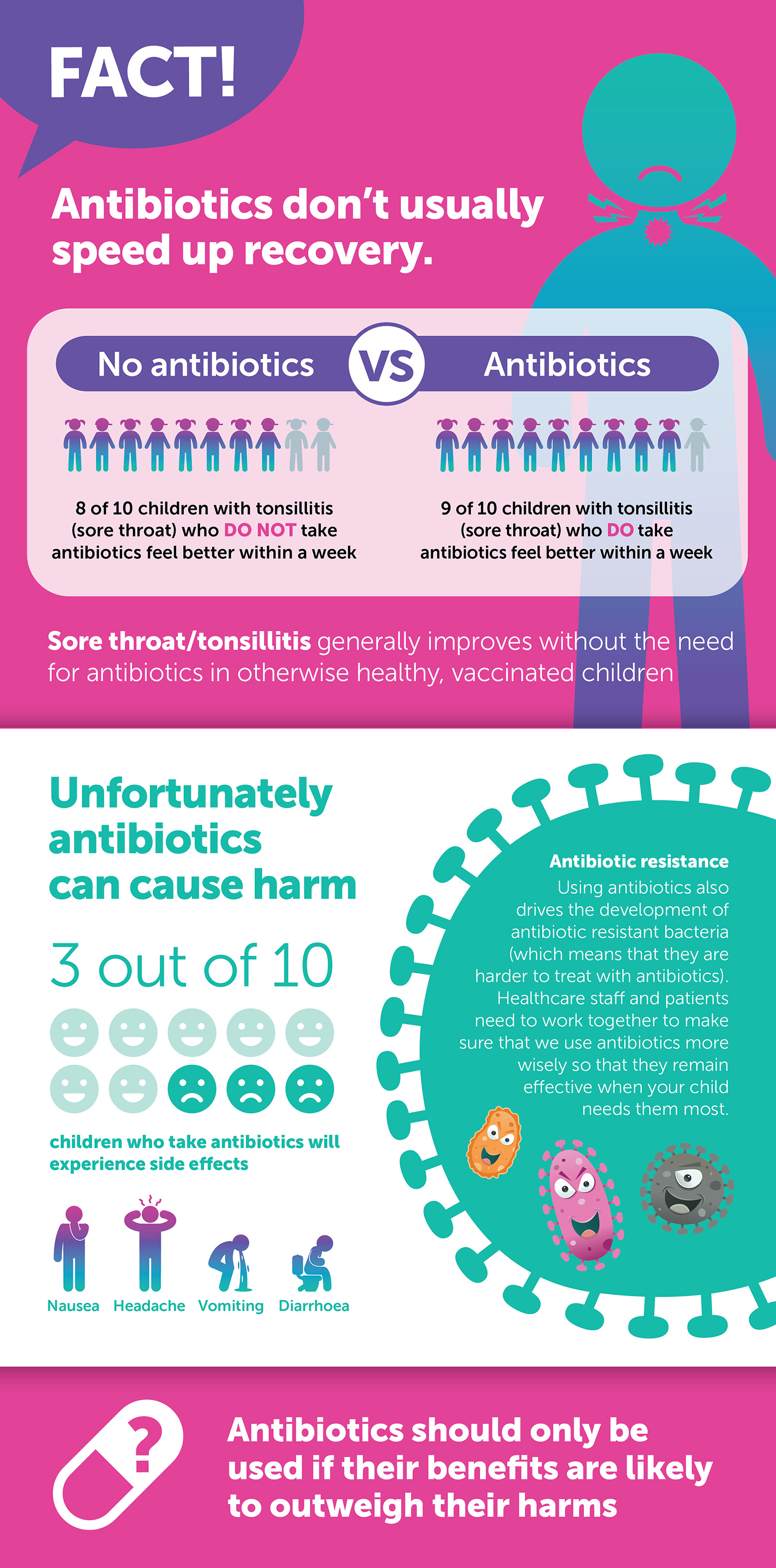
- Viral infections tend to get better on their own and do not need treatment with antibiotics. Antibiotics may actually cause side effects such as rash and diarrhoea and can increase the risk of them developing antibiotic resistance